Everyone knows their doctor records a myriad of information that objectively monitors our health. What many don’t know is that data in the form of our Facebook friends, tweets, web surfing history, and credit card purchases can ALREADY be used to predict our future health. Furthermore, more exotic data is becoming available daily through the adoption of wearable devices and our omniscient smart phones. Combining traditional medical information and alternative medical data to create an individualized accurate model of our future health needs is the promise of big data in healthcare. The monumental task of collecting and analyzing all this data has already begun by a smattering of companies and governmental initiatives. On the long road to complete data integration, our first important step is electronic medical record interoperability.
Steadily since the turn of the century, hospitals and physician offices have been moving data to electronic medical records (EMR). EMRs have improved healthcare by reducing clinical errors and improving provider efficiency. However, electronic records are not easily shared among providers (interoperability). In a system where health care is fragmented amongst many specialists, this is large problem. In fact, the current method of sharing data is scarily archaic. When a health care provider wants a patient’s external records the following happens:
1) A request is sent via fax to the facility with the record
2) The record holder prints out the record from their own EMR and faxes it back
3) The receiving party scans the documents, or worse, puts them in a paper file that will never be consulted.
It might be hard to imagine that potentially lifesaving information is so poorly managed when all your other electronic information is never more than a click away.
What is the cost of our poorly connected medical infrastructure? A study by the Center for Information Technology Leadership showed that interoperable medical records would directly save $77 billion a year by reducing unnecessary repeat testing. Furthermore, the subsequent savings through better patient tracking and management is suggested to save between $180 and $320 billion a year. The dollar cost, notably exorbitant, doesn’t capture the delayed diagnosis, improper treatment, patient frustration, and morbidity related to lack of adequate information exchange. Making digital patient information available to all providers should be a simple enough task…
So why don’t we have EMR interoperability in the country already? Chief among the reasons is economic incentive; there just hasn’t been any (…until recently). In a system where all test and procedures generate profit health care providers have no financial incentive to seek existing information. They are more profitable by repeating a test. Health care systems where economic incentives exist have perused interoperability. One notable example is the Veteran’s Association hospital system (VA). The VA runs 1300+ hospitals across the country, caring for over 26.5 million veterans. Since veterans can receive care at any VA hospital and the VA budget is limited, the system has an intrinsic benefit to reducing unnecessary repeat test costs. In 1999, the VA system was the first US system to adopt an EMR that shared medical records, laboratory data, and imaging across all hospitals. That’s right…. 1999!! Luckily the affordable health care act is pushing health care systems into accountable care organizations where there is true profit, and therefore incentive in reducing unnecessary testing, promoting interoperability. So…problem solved? Not quite.
Economic incentive alone is not enough. Single payer countries such as England and Canada included do not have 100% interoperability for all medical records despite large economic incentives. Their attempts have been limited by political hurdles as well as America’s second stumbling block, standards. The numerous EMR platforms out there can’t just swap a file to share records like you would to share a PowerPoint presentation. They lack standardization because the main law regulating health care information, the Health Information Portability and Privacy Act (HIPPA), does not spell out a particular data format. Therefore each existing EMR, be it home grown or large commercial package, uses totally different formats. We are in desperate need for the department of Health and Human services to decree a standard EMR format to ease the transfer of data. I liken our current situation to a world that has recently invented railroads but failed to standardize the track.
The challenges facing interoperability are not unconquerable and progress has already been made. Ideally we want a system that seamlessly transfers all available records of a given patient when they show up for care. A major step toward this goal came out of a consortium of many parties in the healthcare industry. This voluntary group of EMR developers, health care providers, payers, is called eHealthExhange. Their main rule states: “Participating organizations mutually agree to support a common set of standards and specifications that enable the establishment of a secure, trusted, and interoperable connection among all participating Exchange organizations for the standardized flow of information…” alternatively stated: follow our standard format and build a secure interface to your patient data. According to their website, approximately 80 major participant health care systems are now compliant, including some of the largest in the country: Kaiser Permanente, MedVirginia, the VA, and I am happy to say my home institution Stanford University. The eHealthExchange allows for seamless access to health information at any of the partners.
Another method to get clinical data to follow the patient is to simply hand over an updated medical record to the patient. There are several programs that let patients build a personal health record (PHR) by manually entering your conditions then having them available via a web interface or mobile app. Among the leaders in the field are Microsoft Health Vault, Dossia, and various apps (also Google Health offered this service before discontinuing in 2012). The main problem with these systems is that it puts the onus of data entry on the patient, which is extremely error prone and worthless in emergency situations. In addition, use of these PHRs has not been shown to improve any leading health indicator.
As stated earlier the road to big data involves incorporating more than just patient medical records. Your health is the cumulative result of your daily habits. Monitoring those habits could help clinicians and patients suggest personalized interventions to improve long term health. Today, many people are using their smart phones and other wearable devices to monitor their activities. Currently devices record everything from daily exercise, sleep patterns, heart beat anomalies, blood sugar, and even brain function. The possibilities are ever increasing as new devices and apps come to market. According to ABI research, there will be 480 million wearable devices in use by 2018. Most of these devices come with flashy interfaces to visualize recorded data for the user, but again there is lack interoperability. There is no way to see all your collected metrics across a variety of devices. Furthermore, the data generated from these devices is not available to your traditional health care providers. Luckily a number of start-ups have sprung up to unify device data streams and make them more functioning for users and clinicians alike. One particular leader in this field is Validic, a North Carolina based startup. They offer a platform that sits between devices and the health care providers. This platform aggregates all the device information into one place making it accessible to user and physician alike (highlighted by their beautiful promotion material)
 https://validic.com/our-solutions
https://validic.com/our-solutions
By providing an API (application programing interface) for their platform, wearable device developers are saved the trouble of making their own interface to the numerous EMRs. By building just one Validic supported interface they instantly become accessible to multiple EMRs!
But with all great technologies…there are multiple people working the same idea. HumanApi a Palo Alto based startup also offers a way for health care systems to integrate the vast volume of device generated data in a meaningful way. They also provide an API for developers and an interface for health care providers to monitor and curate patient generated data. (Also their schematic is simpler!)
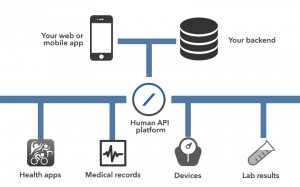 https://docs.humanapi.co/docs/architecture
https://docs.humanapi.co/docs/architecture
Both companies could leverage their patient generated data streams to build the next generation of personalized health care solutions. In addition they will help bring devices and apps from fun gadgets to true meaningful impact, bringing us closer to the much talked about “monitored life.”
All in all we are in a promising time in healthcare. The human genome, completed just over decade ago, is just starting to give up its secrets. In that time we have learned about the transcriptome, epigenome, and microbiome which are equally important to determine the programming of the human body. Combining information from wearables (and eventually invisibles) with the knowledge gained through basic science research we will gain a more complete understanding of the human condition; and how to improve it. As a doctor and a researcher I am thrilled at the possibilities and hope I can convey my passion to you (along with a little education).
I hope you have enjoyed reading my inaugural blog article. If you have any thoughts about the article please feel free to share them in the comments or contact me. Likewise, if you have any suggested topics or interesting innovations to share please get in touch.